The surgical scope of this practice literally runs from the esophagus to the colon and all the structures in between. Dr. Gillian has personally taught courses involving laparoscopic surgery on nearly every organ in the abdomen and every hernia type. Consequently we are comfortable with the surgical evaluation of any intrabdominal organ or structure particularly when chronic pain is an issue. The technical expertise we have allows us to do this safely and typically in an outpatient setting
We are often asked to see patients that were originally evaluated in Primary Care, Pain Management, Ob/Gyn, Urology and even other General Surgical practices for their pain but without resolution. The lack of improvement prior to seeing us is not typically due to a lack of effort on the part of the patient or clinician. In fact, the patient typically brings us a pile of notes and imaging studies to review. The typical limiting factors are often the comfort level of the prior physician with evaluating the patients complaints surgically or being confident that they can fix the issue when found. This often required division of scar tissue or working in areas where the anatomy has been altered by prior surgery.
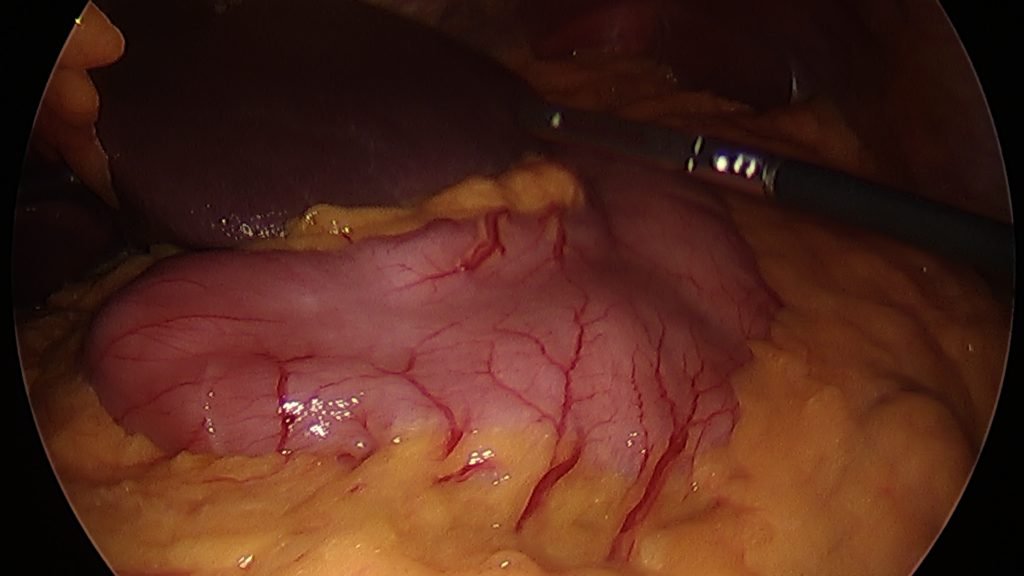



During a diagnostic laparoscopy we are also able to evaluate the entire length of the small intestine to look for scar, inflammation, signs of obstruction, and abnormal lymph nodes. Any abnormalities can be documented, biopsied if need in in many cases resolved during the same procedure. All of these efforts can be accomplished in an outpatient setting with 5mm instruments and same day discharge.
During a diagnostic laparoscopy we are also able to look at the diaphragm,distal esophagus, stomach, duodenum, liver, gallbladder and spleen when we are searching in the upper abdomen. This can all be done with 5mm instruments and adhesions can be divided and biopsies of any abnormal tissue taken.
Once the small intestine is evaluated we are able to turn our attention to the large bowel ( colon) , appendix and pelvic structures. We are often able to find undiagnosed hernias in the groin, ovarian cysts, scar to the abdominal wall from diverticulitis and even endometriosis.
Not every patient with chronic abdominal pain will need or even benefit from a surgical intervention. It is always a judgment call about risk vs. benefit when we choose to operate. However these decisions are based on a history of caring from hundreds of patients in the past with similar problems. Consequently we are able to be more confident that our interventions will either decrease the pain or safely eliminate incorrect assumptions about what may be causing it.
