Laryngopharyngeal Reflux is a highly descriptive name for a poorly understood problem. At first glance even the name creates a link between the pathology and symptoms and makes obvious sense. If you reflux into your larynx or “voice box” you should have problems with your voice. If you reflux into your pharynx or that zone where your swallowing tube and breathing tubes are one and the same then you may have a chronically sore throat. Consequently you will be trying to clear your throat constantly and may event feel like there is always something there – a “lump in my throat” or globus as we call it in the medical world. In more severe case refluxed fluid and debris could fall into the breathing tubes ( trachea) and create a repetitive cough. This cough can even be mediated just by chronically irritating the nerves in the upper airway and pharynx without actually aspirating the debris into the lung.
So… this seems to be a strait forward situation. If you stop reflux into the upper airways then all the problems detailed above should stop. Why then is this such a difficult diagnosis to make? Why is it so difficult to manage once it is suspected? Why are the results of treatment or even surgery so difficult to predict? Why do we call it “Silent Reflux” when reflux doesn’t exactly make “noise”.
ENT and General Surgery Perspectives
LPR is difficult to treat because so many specialist are involved in the patients care and there is no consensus about the definition of the disease or the treatment. It is not unusual for a patient to have seen a Primary Care physician, a Pulmonologist, an Allergist, and ENT, a Speech Pathologist or even a “alternative medicine” specialist before arriving in our office. The presenting scenario is typically sore throat, phlegmy throat, hoarseness, non-productive cough and a lack of response to anti acid medications, inhalers, steroids and dietary change.
Prior to arrival in our office patients have typically undergone a variety of procedures including: endoscopy, bronchoscopy, flexible laryngoscopy, CT scans of chest and sinuses, Chest X-rays, Allergy testing, barium esophograms with speech pathologists. Typically mild to minimal findings are noted but lack of response or minimal change to attempted therapy is typical.
ENT doctors are typically involved in the evaluation of patients with LPR prior to their arrival in our office. This web site provides a wealth of information about non-surgical management and evaluation of LPR that I think every patient should be aware of prior to having anti-reflux surgery.
Once non-reflux related issues have been appropriately addressed by other clinicians we become involved. Unlike our more “Classic” heartburn and reflux cases, people with LPR do not describe these issues as being a predominate problem. This is confusing to clinicians who do not deal with LPR. They presume that a patient must first have pain, damage or heartburn symptoms involving the distal esophagus before it can reach the upper esophagus to cause symptoms in the larynx, pharynx or lungs. They also presume the issue is distinctly an acid problem.
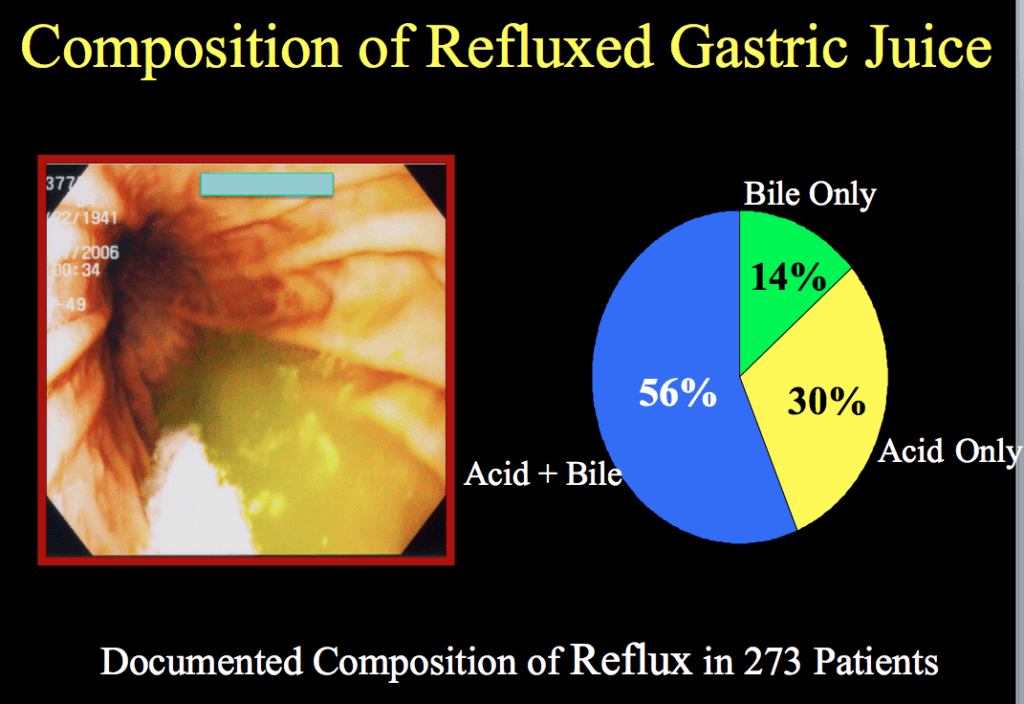
The reality is that the proximal airway and esophagus are very sensitive to minimal episodes of irritation. So it doesn’t take as much refluxate to provoke a response – cough, swallowing, cough, phlegm or mucous production. It is also important to note that we are refluxing a variety of substances from our stomach not just acid. Bile, Enzymes and the food you ingest is not changed by the proton pump inhibitors or anti acid medications your are taking but they are irritants to your larynx and pharynx.
If we are able to demonstrate proximal reflux of any kind into the proximal esophagus in a patient that has not been responsive to medical management of GERD,Asthma, Allergies, and Sinus issues they may be a candidate for anti-reflux surgery because it is the only way to actually stop or severely curtail the reflux of all types of fluids from the stomach into the proximal esophagus.
Best definition of LPR I have ever seen:
“…anything that comes up from the esophagus to the larynx resulting in pathologic behavior, sensation, or findings.”
Dr. Christopher Chang, Fauquier ENT from a meeting of the American Society of General Surgeons in 2013.
LPR symptoms may include any combination of the following. Each can vary widely in intensity.
- Water Brash
- Heartburn
- Phlegmy Throat
- Chronic Cough
- Hoarseness
- Globus – “lump in throat”
- Chronic Throat Clearing
- Vocal Cord Dysfunction
There are many other conditions that may create symptoms that are confused for LPR and must be considered prior to any surgical interventions
- Eosinophilic esophagitis
- Pertussis ( Whooping Cough )
- Strictures in the esophagus
- Vocal Cord lesions or polpys
- Laryngeal Sensory neuropathy
- Muscle Tension Dysphonia
- Psychogenic Globus Pharyngeus
- Allergies or Dietary triggers
- Auto-immune Disease
- Esophageal Motility Disorders






